Update
(Page 3)
Gastrointestinal Bleeding and Hemoglobin
Waiting for a surgery date, I continued with my daily routine, always conscious about my condition. During the week it was all about work, but on Friday and Saturday nights, I would venture out with my friends to a club or bar with a live band for a bit of socializing and dancing. Years ago I discovered drinking everyday took away the fun on the weekends, so ever since I limited my libations to weekends only (meaning, no alcohol from Monday through Thursday).
So imagine my surprise when on February 1, 2020, I ended up in RCH emergency with Gastrointestinal Bleeding. It was Saturday afternoon and I was helping my sister with her kitchen counters when I began feeling nauseous. Thinking it was something I ate, I went to the bathroom and discovered my stool completely black. I would spend the next six days in the hospital being injected with IV’s, blood transfusions, plasma, and a bunch of other medications because my Hemoglobin had dropped below 80 g/L (the normal range being 135 g/L to 170 g/L).
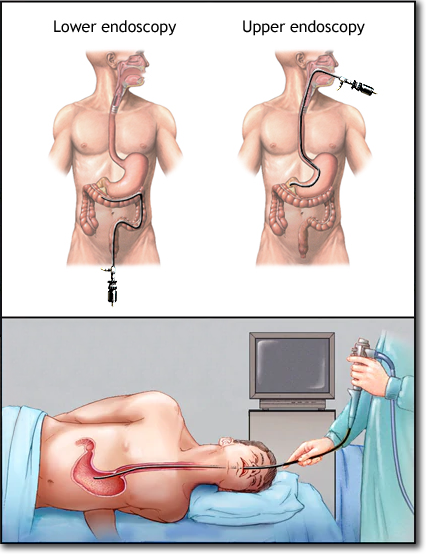
Through upper endoscopy they confirmed my bleeding occurred in the esophagus near the stomach area, and hence why my stool was completely black (the blood turned black because it traveled through my entire intestine). If the bleeding was in the lower intestines, the stool would have been bloody and red in color.
So the $64,000 question was: Why the Gastrointestinal Bleeding?
It was suggested that alcohol was the cause, but a few beers on the weekend could not have been the only culprit. Out of fairness, I have to concede it might have been a contributing factor, but one cannot rule out all the medications, especially the anticoagulants, I was on. For the last ten years I had been alternating daily between 3mg and 4mg of Warfarin to maintain my 2.5 to 3.5 INR range. Along with Warfarin, I was also taking ASA 81mg Aspirin, and because of my stents, I was on Plavix for a year when the GI bleeding occurred.
I’m no conspiracy theorist, but one has to wonder if all that anticoagulant prevention medicine flowing through my veins eventually had some adverse effects, making my arteries and intestine walls malleable, pliable, and inadvertently changing their surface composition. Not unlike anticoagulant rodenticides used in rat poisons to interfere with Vitamin K activation and eventually cause internal bleeding and death, it’s not unreasonable to speculate that ingesting smaller quantities of anticoagulants over longer periods of time could also harm a human body. I see each doctor working in their own world, prescribing their own specific medicine for the area of need, but there is a ‘big picture’ that no one seems to address: all these medications don’t just solve one specific problem — they all have side-effects, and each can affect the body/each other in adverse ways.
Have you seen the big Pharma drug commercials on TV? Every drug ad states its purpose, before spending the next few minutes listing the possible side-effects. Back in the day, there were tiny lines of print at the bottom that no one could read, but now they boldly tell you about the potential risks with a calming, trustworthy, don't-give-it-a-second-thought voice, as not to sound alarming. If a product solves one problem, but may be responsible for multiple side-effects, it stands to reason that combining multiple drugs will only exacerbate that potential. Understanding how some drugs are tested and realizing the seriousness of their side-effects years down the road (i.e. FenPhen) is a discussion for another time, but needless to say, a hodgepodge of chemicals/drugs absorbed into your system is never without consequences.
Apparently I was not the only one who saw this, because while in the hospital I was immediately taken off of ASA and Plavix, and haven’t had a problem since. The downside was now I had to take Pantoprazole T 40mg daily (used to treat damage from gastroesophageal reflux disease (GERD), and in my case, gastrointestinal bleeding) for the rest of my life.
The best news, though, came from Dr. Wong during my surgery consultation. Because of my valve type — the On-X valve — I should have been taking much less Warfarin for the past ten years. About half less — or 2mg every day, to keep my INR range between 1.5 and 2.0. Less Warfarin meant less anticoagulant in my body, less bleeding if I got cut, and possibly less problems in the future because I was no longer ‘overdosing’ on the drug. I only wished someone said something years ago, rather than treating my On-X valve like an older, less efficient model. Perhaps I could have avoided many a complication, including the gastrointestinal bleeding.
Did I mention I’m against drugs? — recreational or otherwise
