Diagnosis
(Page 8)
The Last Supper
On August 26, 2010, the day before my surgery, I was transferred to VGH in the early afternoon. The intra-hospital Ambulance paramedics carted me through the hospital maze before arriving at my destination — a single occupancy room in the Cardiac Ward.
Within minutes the nurse on duty walked me through the Do’s and Don’ts of surgery preparation: I was not to eat anything after midnight, take a shower, rub down my entire body with sterilized wipes, and do the entire sterilization again first thing in the morning to prevent bacteria from causing infections during the operation.
After 10 days in the hospital, I had plenty of time to familiarize myself with the medical terminology and procedures that I was about to undergo. Despite all the answers I found on the Internet, there were still outstanding questions, and my first crack at someone directly involved with the operation was with Brett G. Fitzmaurice, the anesthesiologist who would be putting me under. We went over his list of questions/answers and the ‘Release of Responsibility’ paperwork, but the intricacies of my surgery, including the specific procedures, would have to wait until I met with the surgeon.
His name was Dr. Ahmad Poostizadeh, from St. Paul's Heart Centre, and he showed up an hour after the anesthesiologist. He specialized in Adult Cardiac Surgery, and was the next surgeon in line for my valve replacement operation. After introducing himself, he explained in detail what I was about to undergo. Confident, courteous, and professional, I found his bed-side manner comforting, with our conversation taking over an hour as I peppered him with my questions.
Questions for Cardiologist/Cardiothoracic Surgeon:
- How many years do I have left if not operated on now?
- How bad is my Aortic Valve and Aneurysm? How badly calcified is the valve? Does the aneurysm extend into the aortic arch or is it limited to the ascending aorta?
- Is Bicuspid valve a genetic condition? Or could degeneration be a result of eating habits/old age, etc.?
- What do the final tests show? Is it definitively the aortic valve and the ascending aorta that are the issue?
- Can my Aortic valve be repaired? If not, why? Is it too calcified?
- Preferable choice of treatment for me (47 years of age) for a valve and aneurysm repair: 1) Ross Procedure? 2) Live tissue valve? 3) Mechanical valve?
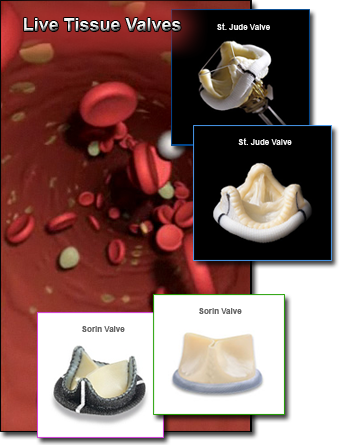
- If 'mechanical valve' used then what brand? St. Jude, Sorin Group, etc.?
- If 'mechanical valve' used then will Dacron (graft) be used along with a mechanical valve or will it be 2 pieces?
- How long will the mechanical valve last realistically, given that I take/monitor Warfarin as prescribed? 15 years? 30 years? Lifetime? Are there any studies that give statistics?
- If mechanical valve, what are the drawbacks? Take Warfarin forever? Check dose every day?
- Does the mechanical valve make noise? How prominent will it be? Will I hear it at night when quiet and sleeping?
- Can procedure be done using the minimally invasive aortic valve replacement technique (5-7cm incision) as in University of Maryland Medical Center?
- Will I lose enough blood during surgery to require a blood transfusion?
- Will there be pictures/video taken of the procedure? Can it be arranged?
- Will the valve be saved for analysis? Can I keep it as a souvenir?
- How many people are involved with the surgery? One surgeon only?
- How long will the operation take? 4 hours minimum?

As we worked through the questions, the scope of the operation and the many options I was facing finally narrowed down to a few. One of the biggest questions I struggled with for days was the choice between a mechanical vs. live tissue valve. Could I live with the constant ticking noise? Would I be comfortable taking blood thinners for the rest of my life?
But after speaking with Dr. Poostizadeh, the answer was obvious. Live tissue valves had an average life span of 8-15 years, depending on your age and active lifestyle. This meant I would need another open-heart surgery to replace the valve in 15 years, and that was not an option.
My only surprise that night was the valve itself. I had rigorously researched two manufacturers of mechanical valves — St. Jude and The Sorin Group — who seemed to dominate the Internet articles. But to my surprise, Dr. Poostizadeh recommended On-X valve from a company called On-X Life Technologies, Inc. This was the first time I heard the name On-X, but I was excited to learn more about this ‘new kid on the block’. With a bit of research, I came across the manufacturer’s website, On-X Heart Valves, that showed the valve to be not only more advanced than its competitors, but potentially requiring less anticoagulation medicine. And that was music to my ears.
When my consultation with the surgeon came to an end, I felt quite comfortable putting my life in his capable hands. He was direct without sugar-coating the facts, and honest enough to disclose that only during surgery could he determine the best course of action to correct my aortic valve and the ascending aorta aneurysm. CT Scans, x-Rays, and Echocardiograms could only show so much, with the true picture of my internals to be unraveled during surgery.